Current Updates (as of 10/31/23)
|
Past Updates
Medicaid Reform
The February 9, 2015 meeting of the North Carolina legislative Program Evaluation Oversight Committee did not include a vote on the Medicaid reform bill to establish an independent board within the Department of Health and Human Services to oversee the state’s Medicaid program. The proposal was omitted from the meeting agenda; and the panel is awaiting additional information. (Source: HMA Weekly Roundup, 2/11/2015)
Managed LTSS Program
In April 2005, DHHS and PBH began operating a pilot program in five counties, under §1915(a) authority, for the delivery of services to individuals with mental illness; I/DD; and substance abuse disorders. In 2011, new state legislation required North Carolina DHHS to restructure management responsibilities for the delivery of these services through a §1915 (b)(c) MH/DD/SA Waiver. Since April 2013, the state’s entire MH, DD, and SA system has operated under the §1915 (b)(c) MH/DD/SA managed care waiver. Under this waiver, the state’s Local Management Entities (LME’s), which once coordinated and offered publicly supported behavioral health care services, have become managed care organizations (MCO’s). (Source: State §1915 (b)(c) Waiver Information website; DHHS §1915 (b)(c) Waiver website; NC Medicaid Reform Proposal, links no longer available 3/17/2014)
On March 17, 2014, the state released a detailed report of the Medicaid reform proposal the state Medicaid department recently submitted to the state legislature. Under Session Law 2013-360, the state DHHS was required to develop a detailed plan, known as the Partnership for a Healthy North Carolina, to reform the state’s Medicaid program. The proposed plan will not pursue a traditional risk-based Medicaid managed care model. Instead, the proposal will: 1. Establish provider-led Medicaid ACOs for the management of physical health; 2. Continue the consolidation and strengthening of the Local Management Entity Managed Care Organizations (LME-MCOs) providing services for the mental health, substance abuse, and I/DD populations; and 3. Streamline and strengthen the coordination of Medicaid LTSS. The legislature is expected to vote on the proposal as early as May 2014. (Source: HMA Weekly Roundup, 3/19/2014) NC Medicaid Reform Proposal, link no longer available (3/17/2014)
On May 29, 2014, WRAL/NC Capitol reported that the North Carolina Senate released its Senate budget proposal, which includes $4.9 million to create a new Medicaid center to oversee the state’s Medicaid program in order to move the program out from under the state DHHS agency. The proposal also aims to dismantle CCNC and dramatically reduce Medicaid eligibility for the aged, blind, disabled, and medically needy, cutting off medical care to around 15,000 current recipients, many of whom are in assisted living and LTC facilities. (Source: WRAL/NC Capitol, 5/29/2014)
Draft Senate Bill 744 (5/15/2014)
On June 18, 2014, WRAL/NC Capitol reported that the North Carolina House released a Medicaid Reform Bill to the House Health and Human Services Committee. The bill includes much of the language from Governor McCrory’s reform plan, which was based on developing ACO’s to manage care of Medicaid patients. Under the House bill, providers would form organizations that would lead the Medicaid reform effort. The bill also calls for capitation of payment per Medicaid patient and tasks DHHS with developing the plans for Medicaid reform. (Source: WRAL/NC Capitol, 6/19/14; HMA Weekly Roundup, 6/25/2014)
Draft House Bill 1181 (5/22/2014)
On July 2, 2014, after a lengthy budget impasse, the state House and Senate settled on Medicaid figures for the state budget: $136.5 million for FY 2013-14; and $186 million for FY 2014-15. Other than the budget numbers, everything else in the two proposed budget bills, including potential Medicaid eligibility cuts, is still on the table for negotiations. (Source: WRAL/NC Capitol, 7/2/2014)
As of July 29, 2014, NC lawmakers have not forged a deal over the long-term structure of the state’s Medicaid program. The plan passed by the House would give local doctors and hospitals incentives to create ACO’s to care for the state’s Medicaid population for a set fee. The plan passed by the Senate would look to out-of-state managed care companies to care for the state’s Medicaid population. Additionally, the Senate is pushing to restructure Medicaid and move it from NC DHHS into a new state agency. Either approach would be a major restructuring of the state’s Medicaid program. It is unlikely NC lawmakers will come to an agreement before the legislative session ends on August 2nd; therefore, the legislature may reconvene for a special Medicaid session, potentially after Election Day in November 2014. (Source: WRAL/NC Capitol, 7/29/2014)
On August 20, 2014, the North Carolina General Assembly adjourned, leaving behind the Medicaid reform bill. The Medicaid reform effort will have to wait until the next legislative session begins in January 2015. (Source: WRAL/NC Capitol, 8/20/2014)
On September 24, 2014, the Charlotte Observer reported that state lawmakers plan to continue discussions about a possible state Medicaid overhaul before the General Assembly reconvenes early next year. (Source: HMA Weekly Roundup, 10/1/2014)
During an October 6, 2014 committee meeting, North Carolina lawmakers heard from the Medicaid directors of Virginia, Florida, and Ohio in an attempt to learn how other states run their Medicaid programs. The state directors emphasized the differences between state Medicaid programs and touched on common themes: change should be slow; and all stakeholders should cooperate on making changes. (Source: North Carolina Health News, 10/7/2014).
On June 23, 2015, the News & Record reported that the North Carolina House passed a bill that reforms the states’ Medicaid system by instituting a capitated managed care payment mechanism that would be paid to provider-led MCOs. The bill differs greatly from the Senate’s Medicaid reform plans, which would require insurance companies to enter the managed care market as well. The two chambers will seek a compromise. (Source: News & Record, 6/23/2015)
On August 20, 2015, North Carolina Health News provided an update on the ongoing debate between the North Carolina House and Senate regarding reforming the states’ Medicaid program. The debate centers around transitioning the program to incorporate a capitated managed care model, but the two houses of the legislature disagree what form it should take. The most recent Senate proposal includes—for the first time—a carve out for dual eligibles, meaning that those individuals would remain excluded from managed care. Dual eligibles are routinely among the most expensive individuals in Medicaid programs, largely due to LTSS utilization. (Source: NC Health News, link no longer available 8/20/2015)
The North Carolina legislature, after months of back-and-forth between the two Houses, has passed a compromise bill—Medicaid Transformation and Reorganization (House Bill 372)—that is set to revamp the state’s Medicaid program. The bill was officially signed into law on September 23, 2015. In summary, the state will move to a capitated managed care program. The bill includes the following:
- Establishes the Division of Health Benefits under the state Department of Health and Human Services (DHHS) to administer the program;
- Permits both commercial MCOs and Provider Led Entities (PLEs) to provide services, including long-term services and supports;
- Excludes dual eligibles from the managed care program but the Division of Health Benefits is to explore ways to incorporate dual eligibles in the long-term and report back to the Joint Legislative Oversight Committee on Medicaid and NC Health Choice by January 31, 2017;
- Authority to award three statewide contracts with either MCOs or PLEs, and up to ten regional contracts with PLEs; and
Risk-adjusted growth rates must be 2 percent below national Medicaid spending growth, and plans must meet a medical loss ratio (MLR) of 88 percent. (Source: HB272, link no longer available 9/23/2015)
|
On March 1, 2016, the North Carolina Department of Health and Human Services (DHHS) released a draft version of its Section 1115 Waiver Application which aims to improve the state’s Medicaid program in terms of access, quality, and cost control. The waiver has four major goals, including:
North Carolina’s Section 1115 Waiver will allow PHPs to provide long-term services and supports (LTSS) to Medicaid-only beneficiates, which will include all state plan LTSS services, institutional care, and waiver services available through the states two section 1915(c) waivers. The enabling legislation for the 1115 Waiver, SL 2015-245, instructs DHHS to establish a Dual Eligibles Advisory Committee to formulate long-term strategies to cover dual eligible individuals through capitated PHP plans. DHHS’ hypothetical timeline for the application is as follows:
|
DHHS notes that this timeline is tentative, and is based off an assumed approval date of January 1, 2018 by CMS. (Source: Draft Waiver Application, link no longer available 3/1/2016)
On June 1, 2016, the North Carolina Department of Health and Human Services (DHHS) submitted its Section 1115 demonstration waiver application, which aims to improve budget predictability, quality, efficiency, and delivery system reform of the state’s Medicaid program. The 1115 application includes the implementation of managed long-term services and supports (MLTSS) for Medicaid-only beneficiaries, with the goal of deferring or averting institutional placement. (Source: Press Release 6/1/2016; 1115 Application 6/1/2016)
The North Carolina Department of Health and Human Services (DHHS) has released a detailed design plan for Medicaid managed care that includes the implementation of capitated Prepaid Health Plans (PHPs). The program aims to:
- Create an innovative, integrated, and coordinated delivery system;
- Support beneficiaries and providers throughout the transition;
- Increase access to care;
- Enhance quality and value;
- Establish relations for success.
The new program will be a significant transformation of North Carolina Medicaid, which has primarily been characterized by fee-for-service (FFS) and a primary care case management (PCCM) system. The state now intends, over a lengthy timeline, to enroll as much of 90 percent of its Medicaid population into managed care. Managed care in NC was traditionally limited to a subset of behavioral health and I/DD services provided via capitated arrangements with Local Management Entities – Managed Care Organizations (LME-MCOs).
Beginning in July, 2019, NC DHHS intends to contract with two types of PHPs: commercial plans (CPs), which must be statewide, and regional, provider-led entities, or PLEs. DHHS will award three commercial plans as required under state law, and has also divided the state into six different regions for PHPs to manage. Upon legislative approval, CPs and PLEs will be able to offer two different types of plans, standard plans and tailored plans.
- Standard plans – will serve the majority of Medicaid recipients, and will integrate physical and behavioral health, as well as pharmacy services.
- Tailored plans – will serve particular populations, including behavioral health, and I/DD.
Initial implementation of managed care will exclude the following populations:
- Dual eligibles;
- PACE participants;
- Medically needy individuals;
- Individuals only eligible for emergency services;
- Presumptively eligible enrollees;
- Health Insurance Premium Payment (HIPP) enrollees.
DHHS proposes a phased-in timeline for enrolling additional special populations into managed care over time, including:
|
Certain Medicaid and NC Health Choice enrollees with a serious mental illness (SMI), a substance use disorder (SUD) or I/DD diagnosis as well as those in the TBI waiver; |
Two years after implementation date |
|
Medicaid-only long-stay nursing facility residents (nursing facility stays under 90 days are covered immediately under the implementation); |
Four years after implementation date |
|
Medicaid-only Community Alternatives for Disabled Adults (CAP/DA) waiver enrollees; and |
Four years after implementation date |
|
Dually eligible beneficiaries. |
Four years after implementation date |
DHHS intends to pursue funding for a managed care ombudsman that would provide oversight, monitoring trends, and working to proactively address enrollee issues. (Source: Proposed Program Design 8/2017)
On October 10, 2017, the Winston-Salem Journal reported that North Carolina’s Health secretary informed state lawmakers that the state is on track to submit a waiver request to CMS that will substantially alter the state’s Medicaid program by enrolling as much as 90 percent of the Medicaid population in managed care. The plan, released in August of 2017, was detailed in depth in the September edition of the State Medicaid Integration Tracker.© (Source: Winston-Salem Journal 10/10/2017)
On November 20, 2017, the North Carolina Department of Health and Human Services (DHHS) submitted an amendment to its section 1115 waiver, originally submitted to CMS in June 2016, which seeks to implement managed care for large portions of its Medicaid population, including Medicaid LTSS. DHHS’ tentative timeline for implementation is as follows:
- Request for proposals (RFP) for prepaid health plans (PHPs) – April 2018;
- PHP proposals due – June 2018;
- PHP awards – October 2018;
- Commencement of managed care – July 2019;
- Launch of behavioral health (BH) and I/DD tailored plan, and phase-in of Innovations and TBI waivers – July 2021.
Under the demonstration, all LTSS services, other than PACE and behavioral health and I/DD services provided by LME/MCOs, will be the responsibility of PHPs. Dual eligibles will be excluded. North Carolina intends to operate its 1915(c) waivers concurrently with the 1115 demonstration—that is, coverage for these services will be authorized under 1915(c) and the 1115 waiver will allow for delivery of these services via PHPs. As detailed in the September edition of the State Medicaid Integration Tracker, however, the state proposes an extended phase-in timeline for both institutional and community-based LTSS under the plan. (Source: Press Release 11/20/2017; 1115 Demonstration Waiver Amendment 11/20/2017; Behavioral Health and I/DD Tailored Plan Concept Paper 11/9/2017)
The North Carolina Department of Health and Human Services (DHHS) has released a complete list of respondents to the state’s two requests for information (RFIs), one for managed care operations, and the other for actuarial and financial aspects of managed care. Submissions were due to the state by December 15, 2017. Respondents to the managed care operations RFI, totaling 34, included major players in Medicaid managed care, such as Aetna, AmeriHealth Caritas, Molina HealthCare, UnitedHealthcare, and WellCare, as well as numerous local organizations. Respondents to the actuarial RFI included many of the same entities but with 18 organizations submitting responses. (Source: Operations RFI Respondents 12/15/2017; Actuarial RFI Respondents 12/15/2017; NC DHHS)
On March 2, 2018, the North Carolina Department of Health and Human Services (DHHS) released an RFP seeking an enrollment broker that will assist the state with transitioning to Medicaid managed care, which is scheduled to begin July 1, 2019. The independent enrollment broker will assist with individuals understanding Medicaid managed care, choosing a health plan and primary care physician, and navigating the new system. DHHS has also released a new concept paper, which covers managed care benefits and clinical coverage policies. (Source: Press Release 3/1/2018; Concept Paper 3/1/2018)
On May 16, 2018, the North Carolina Department of Health and Human Services (DHHS) released a revised Medicaid Managed Care Policy Paper on prepaid health plans (PHPs) in the state. This paper is the next in a series of policy papers published by DHHS as the state works to implement expand Medicaid managed care, including LTSS, to additional populations and statewide. A more detailed overview of North Carolina’s proposed changes can be found in the September 2017 edition of the State Medicaid Integration Tracker.
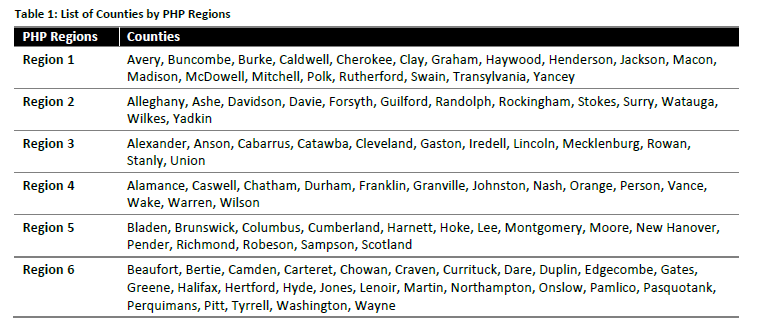
North Carolina intends to contract with eligible PHPs through a request for proposal (RFP) process. PHPs will be one of two types: a commercial plan (CP), or a provider-led entity (PLE). DHHS will set actuarially sound rates for all PHPs selected to contract with the state—therefore, PHPs will not submit price bids as a part of their RFP applications. RFP responses will be evacuated primarily on bidders’ qualifications, and the PHPs proposals to meet contract expectations and requirements. DHHS intends on awarding three PHP contracts statewide, and up to 12 PHP contracts with PLEs for regional contracts. The state has set out six PHP regions, which are as follows:
Beneficiaries that do not select a health plan will be assigned one by DHHS. Contracted PHPs will be held to rigorous monitoring, including financial and quality oversight. Comments on the paper are due to North Carolina DHHS by June 11, 2018. (Source: NC DHHS 5/16/2018)
On October 24, 2018, North Carolina announced that CMS had approved its 1115 waiver application for Medicaid managed care. The waiver approval will allow the state to move forward with implementation of its managed care initiative, including managed long-term services and supports. The approval includes authority for the state to begin implementation. of the base managed care program, known as the “standard plans,” in 2019 and then to tentatively begin implementing specialty “tailored plans” in 2021.
Tailored plans are intended for individuals with a serious mental illness, serious emotional disturbance, severe substance use disorder, intellectual/ developmental disability or a traumatic brain injury. In the interim period before tailored plans are implemented, qualified beneficiaries will continue to be served through the state’s fee-for-service system for primary and acute services and through the existing county-based behavioral health and ID/DD system. Once the tailored plans are implemented, participants will have the choice to be in a tailored or standard plan.
Separately, North Carolina announced that eight vendors submitted applications for the RFP issued in August. The list of entities that submitted applications includes: Aetna, AmeriHealth Caritas North Carolina, BCBSNC – Healthy Blue, Carolina Complete Health, My Health by Health Providers, Optima Health, United Health Care, and WellCare Health Plans. North Carolina indicated that they intend to issue contracts with plans in February 2019 and to begin enrollment on a staggered basis starting November 2019. This procurement is only for standard plans. The state tentatively intends to issue a separate RFP for tailored plans in early 2020.
Sources: North Carolina 1115 Approval Announcement (10-24-2018); CMS Approval Letter (10-19-2018); North Carolina DHHS Stakeholder Update (11-28-2018); List of Offerors (10-19- 2018).
The North Carolina Department of Health and Human Services (DHHS) announced that Medicaid managed care contracts were awarded to AmeriHealth Caritas, WellCare, United Health Care, Blue Cross and Blue Shield of North Carolina, and Carolina Complete Health (regional contracts) as part of the state’s new Medicaid managed care program for 1.6 million Medicaid beneficiaries. The managed care program is expected to launch in November 2019. The program will launch in two phases, the first in November 2019 in 27 counties and the second in February 2020 in the remaining counties. Medicaid beneficiaries who will transition to Medicaid managed care in November will start receiving information on PHPs in June 2019. Phase I participants will select a plan starting July 2019, Phase II participants will select a plan starting October 2019.
The MCOs will be expected to deliver state-plan LTSS services (nursing facility services up to 90 days, home health, personal care, hospice and private duty nursing) to enrollees currently receiving those services FFS. Waiver participants and services will be moved to managed care in later phases of the program. (Source: DHHS Announces Contracts for Medicaid Managed Care, 2-4-2019; Medicaid Managed Care RFP, August 2018)
The state Senate budget proposal included an increase in intellectual/developmental disabilities waiver (the NC Innovations Waiver) slots by a maximum of 1,000. The slots would be made available on January 1, 2020. The bill also includes another increase in slots, up to 1,000 to be made available in January 1, 2021. The addition of the slots would cost $41 million over two years. Services under the NC Innovations Waiver are administered through managed care organizations and other local organizations (called local management entities) to provide LTSS to individuals living in community settings.
(Source: Winston-Salem Journal: 1,000 Slots for In-Home Care; 5-29-2019, NC Senate Bill)
|
The North Carolina Department of Health and Human Services (DHHS) announced the statewide transition to managed care will be suspended. The North Carolina General Assembly adjourned without passing certain appropriations and programmatic authority that DHHS needed prior to implementation. NC Medicaid will continue to provide care for beneficiaries under a fee-for-service structure. North Carolina’s managed care structure was expected to begin on February 1, 2020, but NC DHHS stated they will not announce a new implementation date until they have a budget that supports the managed care program. |
(Source: DHHC Suspends Implementation of Managed Care; 11-19-2019)
On June 30, 2021, NCDHHS announced that the state’s managed care program would launch beginning July 1, 2021. About 1.6 million Medicaid beneficiaries were transitioned into a new managed care plan by May 26, 2021. Participants selected their plan or were assigned a plan. NCDHHS listed benefits of transitioning to managed care which included establishing a value-based payment structure for better health outcomes, the integration of physical and behavioral health, and the improvement of health among Medicaid beneficiaries and the reduction of medical costs by investing in home and community-based services.
(Source: NC Medicaid Managed Care Statewide Launch Press Release; 6-30-2021, NC Medicaid Managed Care Health Plan Assignment Press Release; 5-26-2021)
State Demonstration to Integrate Care for Dual Eligible Individuals (Withdrawn)
In May 2012, the state submitted to CMS a Demonstration Proposal to integrate care for dual eligibles statewide using a managed fee-for-service reimbursement model. (Source: Demonstration Proposal; State Duals Demonstration website, link no longer available) However, in 2013, the state received a §646 waiver expanding the reach of the state’s Community Care of North Carolina (CCNC) program to include dually eligible beneficiaries. Therefore, as of May 2014, the state has withdrawn from the duals demonstration, choosing instead to pursue duals integration through its CCNC program. (Source: National Academy for State Health Policy website, 11/2013; ADvancing States)
Health Homes
In May 2012, CMS approved the state’s Health Home State Plan Amendment for Health Homes targeting beneficiaries with two chronic medical conditions or one chronic condition and at risk for another condition. Enrollment is voluntary through Community Care of North Carolina (CCNC), which provides Health Home services as Medical Homes. (Source: Demonstration Proposal; Kaiser Health Homes website, 6/2014; CMS State Health Homes SPA Matrix, link no longer available 3/2014)

